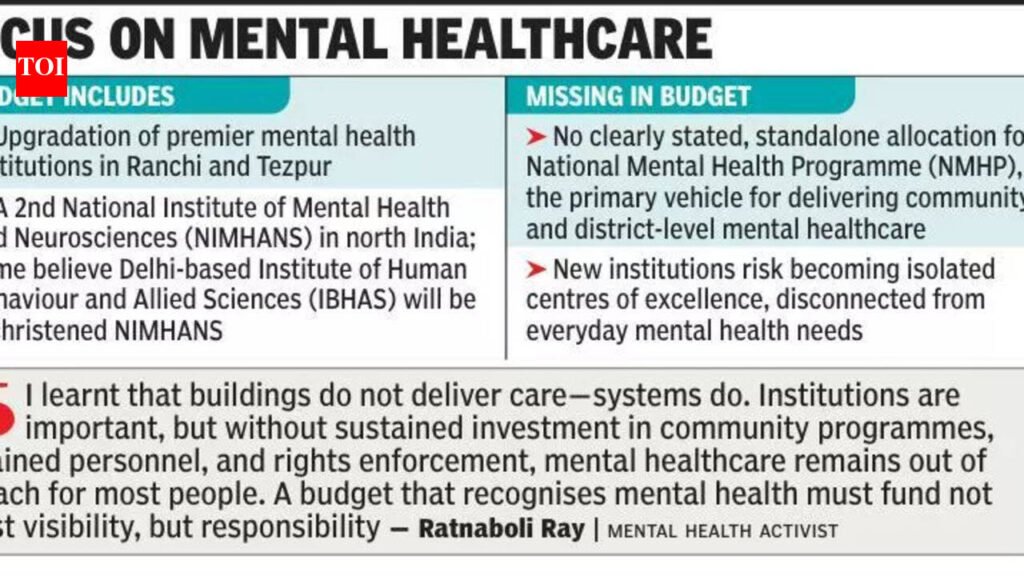
“For most Indians, mental healthcare does not begin at national institutes. It begins at primary health centres, district hospitals, and community services,” she pointed out.Psychiatrist Aniruddha Deb said:”One needs a fine balance between developing centres of excellence and setting up district-level clinics for people suffering from mental health issues.” Institute of Psychiatry assistant professor Prasanta Roy pointed out, “If we study how many productive years are lost due to mental health in India, it will rank higher than most other ailments. For severe mental illness, the productivity loss is long-term. There is scope to prevent mental illness, but most of the stress is on treatment post-illness,” he said.Mental health experts said weak community mental healthcare shifts the burden onto families, especially women, increasing unpaid care work and reducing labour force participation.There is also a governance dimension. Capital expenditure is visible and finite; programme expenditure is ongoing, less visible, and more accountable. “Prioritising institutions over programmes shifts responsibility to states and families, while limiting the Centre’s exposure to rights-based scrutiny under existing laws,” added Ray.